
Going to the doctor is already tricky enough for people with chronic symptoms of Lyme disease. Their concerns often dismissed by mainstream medicine, those patients now face an additional hurdle: ruling out long Covid.
The two illnesses — one seeping in over the course of decades and another suddenly springing to life on a massive scale — share many qualities, including being widely misunderstood. But as efforts to demystify long Covid intensify, so does interest in studying neglected conditions, including persistent complications from Lyme disease.
Long Covid was a crash course in chronic conditions that start with infection. “As a result, Lyme patients are now met with more compassion and understanding than ever in the past. It is now harder for a physician to dismiss the possibility of a Lyme diagnosis out of hand than it was before the pandemic,” said Bernadette Clavier, facilitator of the Coalition for Infection-Associated Chronic Conditions and Illnesses Research.
New studies aim to tease apart the diseases’ differences and similarities in hopes of finding treatments for patients that have gone without vetted, tailored therapeutics, in some cases for decades.
All told, over 10 million people in the United States have long-term symptoms of Covid or Lyme disease, according to recent estimates. Up to a quarter of people treated with antibiotics for Lyme disease go on to develop chronic manifestations, a condition called post-treatment Lyme disease syndrome by the Centers for Disease Control and Prevention. Many others go untreated, leaving the bacteria carried by blacklegged ticks with unfettered access. (While some believe a continuing infection is at play in post-treatment Lyme, others think there’s a different underlying reason for continuing symptoms.)
The condition, like long Covid, can cause a litany of confusing symptoms, like body pain, profound fatigue, and brain fog. And neither group of patients has a clear-cut way of knowing if an infection was the source of their problems.
That’s a real issue for clinicians, says John Aucott, director of the Johns Hopkins Lyme Disease Clinical Research Center. Even to an expert like him, long Covid, post-treatment Lyme and other post-infectious conditions like myalgic encephalomyelitis “all look remarkably similar,” he said. There’s a lot of symptom overlap, and simple blood tests are insufficient to know what the root cause is. In many cases, patients may not have tested for the Covid virus or the bacteria Borrelia burgdorferi that causes Lyme. They may not even recall being sick, or getting bitten by a tick.
“It requires meticulous attention to getting that history and documenting it,” said Aucott, who says multiple of his patients developed long Covid after being diagnosed with post-treatment Lyme. “There’s no shortcuts to it right now.”
That makes getting answers even more difficult. Doctors famously like quick things — tests, scans, biomarkers. Patients in post-infection limbo have no such outs. Sure, there are PCR and antibody tests, including what’s considered the “golden ticket” in Lyme: the western blot, which can detect specific proteins in the blood. People with suspected chronic Lyme often clamor for the blot, thinking it will grant them a sense of medical legitimacy and treatment. But the blot, like Covid antibody tests, taps into the immune system’s memory; it can confirm that a person was exposed at some point, but can’t tell whether someone has long Covid or chronic Lyme, Aucott said.
On the flip side, a negative antibody test could mean a long time has passed since the exposure, or that the test produced a false negative.
Lyme disease is the most common tick-borne disease in the U.S., but ticks can also carry parasites or viruses. Some of those may get caught with standard tests and treated with antibiotics, but not all of them. People may be infected by multiple pathogens at once, or acquire multiple over time. And both Lyme and Covid may make patients more susceptible to other infections, as well as autoimmune diseases.
Researchers are looking for specific biomarkers — and even using machine learning to do so — to distinguish an immune response to, say, a virus versus bacteria. Others are trying to figure out if the body is reacting to lingering virus or bacteria, or just having an overextended immune response to a long-gone infection.
In the meantime, patients and providers are left to sift through a vague set of facts and symptoms and figure out how best to manage a potentially life-altering condition.

‘You feel like you’re crazy’
Almas Eftekhari, a 40-year-old Lyme disease advocate, shrugged off her first, super-mild bout of Covid in August of 2023. The worst of it was losing her sense of taste and smell. But two months later, Eftekhari crashed.
Symptoms she’d attributed to the long tail of her Lyme — diagnosed with a positive western blot after many tick bites in woods near her Northern Virginia home — worsened. Joint pain would migrate unpredictably around her body, and up her neck. Gastrointestinal issues popped up out of nowhere. “Some things are there for three months and they totally disappear. And then you get some new stuff,” she said. ”You feel like you’re crazy.”
Her brain fog got so bad she could hardly form a sentence, much less read a book. Eftekhari said her memory slowed, too. She recalls filling her dog’s bowl with water and forgetting for hours to close the faucet, and needing to buy lanyards to attach her cell phone to her body, because she’d lose it so frequently. Was it Lyme or was it long Covid?
Immune dysregulation can make it so the body keeps fighting a pathogen after it’s been cleared (or at least becomes undetectable on common tests). This chronic inflammation can lead to long-term disruptions in the brain, heart and gut, experts say. Researchers at the Lyme Disease Research Center at Johns Hopkins Medicine observed altered brain activity in the white matter of people with Lyme.
Crosstalk between the immune and nervous systems, mediated by specialized cells, has been found to be altered in monkeys infected with the bacteria that causes Lyme. Neuroinflammation also occurs during Covid, and another monkey study showed aged or diabetic animals fared worse. Other studies have suggested Covid’s “priming” of the nervous system could make people more susceptible to later infections, too.
Eftekhari and her partner, who also has disabling chronic symptoms from Lyme, would argue about it often, she said. “I was like, ‘This is Lyme.’ And he’s like, no, it’s Covid. And I’m like, no, it’s not.”
She was soon thereafter diagnosed with postural orthostatic tachycardia syndrome, or POTS. It’s a condition that can cause, among other symptoms, lightheadedness when going from sitting to standing. The POTS explained the extreme dizziness that flattened her on many days. But also, it’s yet another look-alike syndrome: like long Covid and Lyme, POTS can cause fatigue, cognitive issues, and digestive system problems. Eftekhari wonders if her dizziness isn’t just from babesiosis, a disease caused by ticks infected with a parasite.
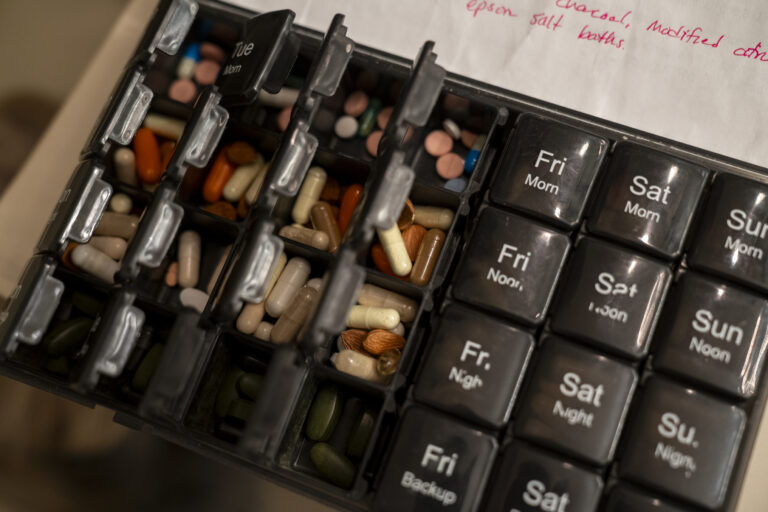
With few treatment options available, Eftekhari has to help herself. She’s trying experimental protocols, mostly consisting of supplements and antibiotics. “I’m hoping that it cures me or at least gets me to a point of remission, but I’m not really sure,” she said.

Antigens and therapy candidates
An elevated immune response can be associated with autoimmune, metabolic, neurological, and endocrine dysfunction, said Beth Pollack, a long Covid and ME/CFS research scientist at the MIT department of biological engineering. Tracking symptoms will help scientists better understand the biology of Lyme and Covid, she said.
Scientists have identified the parts of the pathogens that most strongly provoke immune activation and lead to chronic inflammation. The antigen that triggers the inflammatory responses in chronic Lyme symptoms is found on the outer layer of the bacterial cell wall. The mesh-like scaffolding, called peptidoglycan, is a popular target for antibiotics. This peptidoglycan coats the bacteria and also readily absorbs these drugs. However, pieces of these bacterial cell walls can linger in the body even post infection. This may contribute to the prolonged inflammation that leads to chronic illness. These hidden reservoirs of persistence, in the form of tiny pieces of bacteria that may linger in the neurons or spinal cord, can go undetected because of an inability to test for it.
A similar trend of leftover pathogen pieces in the body may also happen with Covid. While studies have not shown the presence of leftover viral pieces, scientists have concern that these fragments can cause prolonged inflammation.
Detecting the presence of leftover bacterial and viral fragments that can have long-term immune and neurological effects is hard — but identifying a biomarker that reflects chronic inflammation could help. Aucott says immune markers like serum interferon-alpha and the chemokine CCL19 can be useful in research settings, even though they haven’t been validated or accepted as biomarkers by the FDA. Patients are often not tested for these.
Without clear biomarkers, the disorienting overlap between conditions impedes scientific research, some experts say. It will continue to be difficult to tell whether a potential participant in a trial is sick because of long Covid or due to Lyme, or some other condition. Uniformity in study groups will be challenging without knowing all of the triggers participants were exposed to.
“We have to come up with a plan to care for these patients, a plan to do the research that’s needed. It ain’t going to go away,” Aucott told STAT.
There are currently no FDA-approved therapies for chronic Lyme, or full-scale clinical treatment trials — a strikingly similar position to many other chronic conditions, including long Covid. NIH funding for Lyme research has historically been low, but advocates are hoping the spotlight on long Covid will lead to more attention for other chronic inflammatory illnesses. The need is evident in social media support groups, in the sometimes desperate measures patients will take to get some relief. It’s obvious when looking at monthslong waitlists for appointments at clinics specializing in chronic Lyme and long Covid: people need help.
However, there is some movement. Researchers at Johns Hopkins and other institutions have a list of potential new therapies they’d like to study — everything from inflammatory arthritis treatments to antibiotic combination therapies, brain stimulation and magic mushrooms.
Before Covid, the NIH released a research plan that called for greater efforts to understand the cause of long-term symptoms in Lyme disease. Last year, the National Institute of Allergy and Infectious Diseases funded seven research projects into persistent Lyme symptoms, which will run until 2028. NIAID is also trying to design a study to follow Lyme patients starting at the time of diagnosis, to better grasp just how often the disease turned into chronic or recurring symptoms, an NIH program officer said in a recent meeting.
In July, the NIH announced a funding opportunity for research on neurological and psychiatric manifestations of infection-associated chronic illnesses, including post-treatment Lyme and long Covid. It’s one step in the direction of what advocates and some researchers have been asking for: research infrastructure without silos, so murky areas between diseases and body systems can be explored.
It’s possible, Pollack says, that cross-illness trials are a key — one way to decipher and help patients with multiple chronic inflammatory illnesses. These kinds of studies cast a wide net for participants with shared symptoms, and then analyze in-depth the overlaps in their conditions (for example, a long Covid trial with an arm for participants with POTS, and another for ME/CFS patients).
“We need to study the most complex patients, not just the ones who fit into boxes,” she said.
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies. Our financial supporters are not involved in any decisions about our journalism.
To submit a correction request, please visit our Contact Us page.




