Until recently, getting an MRI meant traveling to the hospital. But a new generation of more affordable and highly portable MRI (pMRI) devices are rapidly reshaping neuroimaging research and clinical care. The scanner will now come to you. That means the time is ripe for a related innovation: neuroimaging counseling.
While portable MRI is emerging for many body parts, scanning brains with pMRI raises unique ethical concerns. Portable brain MRI devices could soon be available in previously unimaginable settings, like your home or a high school gym. Greater access to these devices will allow greater use of neuroimaging in clinical care. But this technological evolution may also pave the way for an even more radical reality: individuals seeking scans for reasons other than to detect a potential neurologic problem. We envision a future of regular brain-health “check-ups” via portable MRI devices, public health neurologic screening, population neuroscience research involving millions of participants, and even direct-to-consumer imaging services akin to 23andMe in genetics.
Because brain scans have largely been reserved for people with brain-related health concerns and participants in neuroscience research studies, most people have never had their brains scanned. But demand has been growing, and as access increases and costs drop, the number of brain scans performed each year could increase by orders of magnitude. There is burgeoning interest in whole-body MRI scanning, for instance, buoyed by popular media coverage and celebrity endorsements.
With the support of NIH BRAIN Initiative grants on portable MRI and community engaged MRI research, we’ve been tracking these developments. And our findings raise concerns about who is going to explain to people who have these scans what they mean?
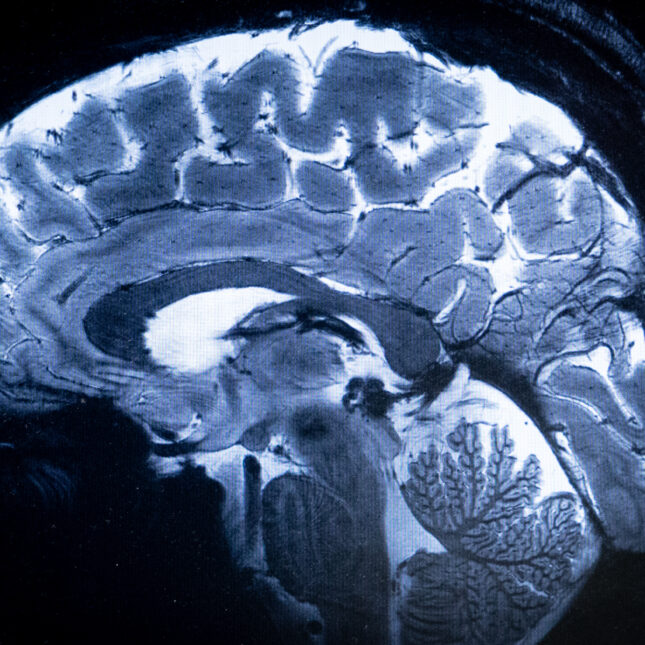
MRI scans offer a tremendous quantity of complex information. In addition to generating findings related to major neurologic pathology, like a new brain tumor, they often also detect abnormalities of unclear significance. Often described as “incidental findings” (or incidentalomas) because they are not the main purpose of the scan, these abnormalities generally come as a surprise, because they have typically not had an impact on an individual’s health or quality of life. Their appearance on an MRI, however, suddenly raises questions about what, if anything, to do about them.
For instance, an MRI might uncover a brain aneurysm (a blood vessel bulging where it has weakened) that might rupture, thus warranting a discussion about the risks and benefit of surgical intervention. Or it might show “white matter disease,” which can be an indication of underlying atherosclerosis and risk of future strokes, or signs of brain atrophy that may be benign, age-related changes or serious neurodegenerative ones.
Understanding what a brain scan shows isn’t like simply identifying abnormal lab numbers on a lab report, a task that average people can do. It takes expert guidance and support to help people wade through complex MRI information and navigate next steps.
Today, physicians and nurse practitioners are the main experts who explain MRI findings to patients. But there won’t be enough of them to meet the looming demand, especially given the lack of pre-existing relationships between physicians and individuals obtaining MRI scans via direct-to-consumer imaging. Even with teleneurology — the use of virtual platforms to provide neurologic care and expertise — there are simply not enough qualified clinicians to meet what will be completely unprecedented demand.
If our prediction of a massive increase in MRI scanning is correct, then the U.S. will need many more experts who can help people understand what their brain scans mean.
This type of dilemma is not new to medical practice. In the 1940s, physicians began discussing the concept of genetic counseling, a discipline that would both provide patients with information about their genes and help them digest the emotional and psychological effects of it. Today there are dozens of masters-levels training programs in genetic counseling and more than 3,500 practicing trained genetic counselors in the United States alone, who specialize in helping patients understand the implications of their genetic results.
To address the coming rise in neuroimaging, we suggest that the field of neuroimaging counseling be created. Like their genetic counseling counterparts, neuroimaging counselors would be trained to help explain neuroimaging findings to individuals who receive brain scans. To be clear, the clinical interpretation of scans would remain in the domains of medicine that traditionally make them: radiology, neurology, and neurosurgery. But communication of those interpretations, addressing follow-up questions, and facilitating dialogue about the emotional weight of abnormal brain imaging results would be supported by neuroimaging counselors. By working with communities to improve knowledge of human neuroimaging research, they would also play an important role in identifying, engaging and enrolling participants with informed consent in research studies. Neuroimaging counselors would also help researchers and clinicians better understand the concerns of patients and communities.
While neuroimaging counseling would in some ways be similar to genetic counseling (for instance, its focus on communicating uncertainty and ambiguity), the two fields would differ in important ways. Neuroimaging counseling would have to address the realities of interpreting a brain scan that represents just one snapshot in time. Unlike genes, which don’t significantly change over the course of a human lifespan, brains are constantly changing, and so an individual’s brain scan will change over time.
Neuroimaging counselors would need to undergo rigorous training programs, perhaps obtaining specific credentialing via accredited master of science programs with curricula covering basic and clinical neuroscience, neuroimaging, ethics, and counseling. We envision that they would work alongside researchers and physicians in both hospital (as a consult service) and outpatient settings, and would also belong to a designated professional society. Similar to genetic counselors, they could be reimbursed via a mixture of insurance coverage as well as out-of-pocket payments.
Neuroimaging counselors could contribute to the clinical and research neuroimaging process in several ways:
- helping consumers and potential research participants make informed decisions about whether to have a brain MRI scan
- addressing pre-scan anticipation and anxiety
- following-up to help explain the resulting findings and their consequences
The precise role of these counselors on the care or research team would have to be carefully outlined, especially given the reality that interpreting imaging results is, to some extent, a subjective practice, even among top neurologists, radiologists, and neurosurgeons.
MRI for all is not happening tomorrow. But it is coming soon. It’s important to take a lesson from the era of AI, in which medicine and other fields are scrambling to catch up to address its ethical and legal challenges. The time is now to plan for the future of neuroimaging. Training a cadre of counselors can help address the emerging challenge of widespread access to brain scanning technology. As a first step, we recommend that an interdisciplinary working group be created to define this new profession and its position in the face of the changing landscape of medical practice.
Nancy Lu is a fourth-year student at Harvard Medical School. Sumita M. Strander is a fifth-year year student at Harvard Medical School. Francis X. Shen, J.D., Ph.D., is a professor of law at the University of Minnesota and a faculty member in its Graduate Program in Neuroscience, a member of the Center for Bioethics at Harvard Medical School, and the chief innovation officer for the MGH Center for Law, Brain & Behavior. Research for this article was supported by grants RF1MH123698 and 1R01MH134144-01 from the National Institutes of Health (NIH) and the National Institute of Mental Health (NIMH). The views expressed here are those of the authors and do not necessarily represent the views of the NIH or NIMH.
LETTER TO THE EDITOR
Have an opinion on this essay? Submit a letter to the editor here.
To submit a correction request, please visit our Contact Us page.










