News that a person in Missouri contracted H5 bird flu despite having no known contact with infected animals or birds — in other words, no evident route of infection — raises pressing questions public health officials are surely scurrying to answer.
The rationale for that urgency is this: An unexplained H5 infection raises the possibility of person-to-person spread of a flu virus that has never before circulated in humans, and to which people would not have immunity. And this with a dangerous flu virus that scientists have long feared could someday trigger a pandemic.
After all, the 2009 H1N1 pandemic was first noticed when two children in California who had no contact with pigs or with each other were diagnosed with flu infections caused by a virus that had previously been circulating in swine.
To be clear, it is far too soon to conclude this infection can’t be linked to some direct or indirect exposure to infected animals or birds, or to some farm product contaminated with the virus.
But there are, as we noted, questions that need to be answered, and the sooner the better. Here are five.
What is being done to investigate the situation?
Word of the infection emerged late Friday when the Missouri Department of Health and Senior Services issued a press release, followed shortly by a statement from the Centers for Disease Control and Prevention; neither provided much information. The CDC statement said Missouri was conducting the on-the-ground investigation to look for the source of the individual’s infection.
Flu experts watching from afar are puzzled by the seeming lack of urgency. They wonder why the CDC hasn’t sent a team to the state, and why health officials waited so long to make the case public. (The CDC cannot of its own accord send a team of investigators; it must be asked for help by state authorities.)
Their concerns add to criticism that the entire U.S. response to the outbreak of H5N1 viruses in dairy cattle has been lethargic; a number of critics have suggested if this outbreak were happening elsewhere, the U.S. would be up in arms about the tenor of the response. The concern is that if the virus, which is genetically wired to infect birds, adapts to be able to spread efficiently among mammals, that brings it a big step closer to being able to transmit among people.
“I would want to see a ‘better safe than sorry’ investigation,” said Marion Koopmans, head of the department of viroscience at the Erasmus Medical Center in Rotterdam, the Netherlands, said about the response to the Missouri case.
For Koopmans, what is being done to crack the mystery of how this person was infected tops the list of questions that need to be answered. “I would want to see a wide net cast here,” she said, such as looking to see if there is any evidence of hidden chains of person-to-person transmission of the virus. It “does not have to be all in the public eye, but I would want to know this is [being] taken up very seriously.”
The fact that the case was only announced publicly two weeks after the individual was hospitalized, and after the person had recovered and was discharged, seems like a missed opportunity to Angela Rasmussen, a virologist who specializes in emerging infectious diseases at at the University of Saskatchewan’s Vaccine and Infectious Disease Organization in Saskatoon, Canada. Local doctors should have been alerted quickly so they could be on the lookout for other such cases, she said.
“If there is human-to-human transmission, it is critical to carry out the [epidemiologic] investigation as rapidly and efficiently as possible, so the choice to drag their feet and give no details about follow up is mystifying and reflects very poorly on both Missouri state and federal epidemic response capacity and practice,” Rasmussen told STAT in an email.
Thomas Peacock would like to know if people investigating the case have or are planning to draw blood samples from close contacts of the infected person to look for evidence of H5 infections that might have gone undetected. Peacock is an influenza virologist at Britain’s Pirbright Institute, which focuses on controlling viral illnesses in animals.
He believes another explanation will eventually be arrived at, but if it turns out this case involved human-to-human transmission, “the U.S. can’t just sit on its thumbs anymore.”
Is this the same H5 virus that is spreading in cows?
The outbreak in dairy cattle has infected nearly 200 herds in 14 states — that we know of. Missouri hasn’t reported any infections in cows. However, farmers in many places have refused to test their cows. So there could be a lot more of the virus in the country than is currently known.
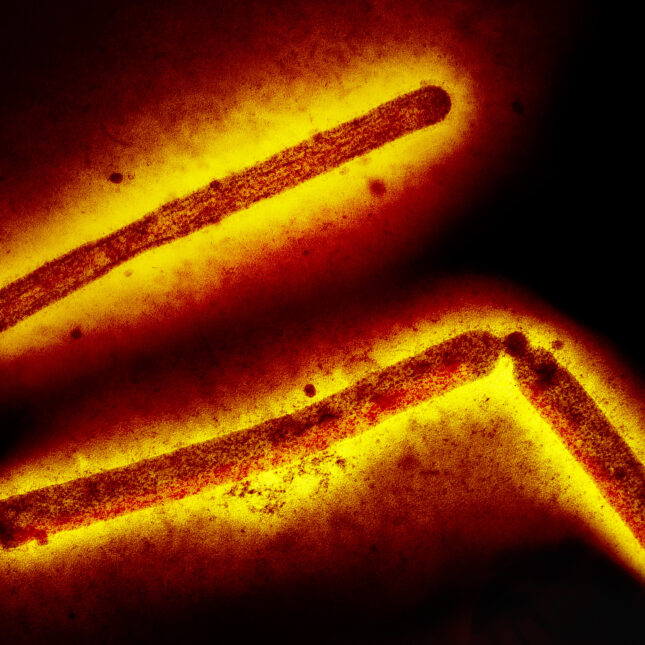
The virus causing the outbreak in cows is highly pathogenic avian influenza — sometimes shortened to HPAI — of the H5N1 subtype. That’s a family of viruses. The specific version in cows is called clade 2.3.4.4b, genotype B3.13.
As of Friday, all that was known about the Missouri case was that the individual was infected with an H5 virus. The CDC was still working to try to figure out the neuraminidase of the virus, the N of its name. Sometimes that isn’t possible, for instance if there isn’t a lot of virus in the sample from the patient.
The CDC is also working to record the genetic sequence of the virus. A sequence could help solve the source of the virus, by allowing a comparison of the virus from the person to other known versions of the virus.
“Honestly, my assumption is it’s going to be high path H5N1. And probably if it is, it’s the bovine one, because there’s just a ton of that out at the moment,” said Peacock.
Rasmussen noted that knowing the N number of the virus is important because influenza A viruses — H5N1 is a flu A virus — can swap genes with each other, creating what are known as reassortants. That process could create a new virus that is better able to infect people, she said.
How sick was this individual? Was he or she hospitalized for influenza symptoms, or for other reasons?
The Missouri press release gives very sparse details about the infected individual, and says that for patient privacy, no additional information will be forthcoming.
The individual who tested positive went into the hospital on Aug. 22. The person had “underlying medical conditions” — though there are no details about how many, and how serious they are. There is no indication of the person’s age, though if it were a child, the press release likely would have said so. It states that the person recovered and was discharged from the hospital. It doesn’t indicate for how long the person was hospitalized or whether any of that time was spent in intensive care.
Why does it matter how ill the person was, and whether it was the flu that prompted the hospitalization or something else? There have been 13 other H5 cases in the U.S. this year, all directly or indirectly related to the outbreak in cows. All of these people had very mild illnesses.
If this individual’s H5 infection was severe enough to require hospitalization, that broadens the picture of the spectrum of illness that 2.3.4.4b B3.13 viruses can trigger. And it would suggest we shouldn’t assume we know how this virus would behave, if it starts to spread among people.
“It is important to know what this [illness] looks like in people, as well as to understand underlying medical conditions that might change a patient’s risk profile,” Rasmussen said.
Did this person truly have no contact with infected animals or birds? Does this individual have a cat that is allowed outdoors?
The press releases issued by the state and the CDC stressed that this is the first H5 case in the country in a person without an occupational exposure to infected cows or poultry. “The patient has reported no exposure to animals,” Missouri said.
But is it possible the person had indirect exposure, for instance, contact with farmworkers who might have been exposed to infected poultry or cows? Some suspected H5N1 transmission events between people in other countries have occurred among people whose close household contacts interacted with infected animals, Peacock noted.
Other experts have questioned whether the individual had bird feeders, which could potentially have exposed him or her to wild bird droppings. They have also wondered whether the household had any cats. There have been a number of reports of infected cats on farms with H5N1-infected dairy cows, assumed to be caused by consumption of infected milk. Cats also could become infected through encounters with infected wild birds.
Did this person consume raw milk?
One of the big questions in social media discussions among scientists this weekend is whether this individual drank raw milk, or consumed raw milk products. Unpasteurized milk from infected cows contains extraordinarily high amounts of the virus. Laboratory experiments have shown feeding contaminated raw milk to mice can induce severe disease. Many of the farms with infected cats have reported deaths among the animals.
It’s not known what risks drinking H5N1-laced milk pose for people but scientists have been worried it could induce disease. Peacock, for one, is surprised that infections linked to raw milk consumption haven’t been identified yet.
“The obvious question I would ask is: Have you ruled out that they’re not someone who’s got a big tub of raw milk in their fridge? Because that just seems like such an obvious route for a cryptic infection,” he said.
Rasmussen agreed that exploring this possibility is critical, saying “if this is [due to] raw milk consumption, this would be very valuable information to have about the feasibility and risk of this exposure route.”






